HUMAN REPRODUCTION
Human reproductive system: organ system by which humans reproduce and
bear live offspring
Provided all organs are present, normally constructed, and
functioning properly, the essential features of human
reproduction are:
- liberation
of an ovum, or egg, at a
specific time in the reproductive cycle
- internal fertilization of the ovum by spermatozoa, or sperm cells
- transport
of the fertilized ovum to the uterus,
or womb
- implantation
of the blastocyst
- the
early embryo developed from the fertilized ovum, in the wall of the uterus
- formation
of a placenta and maintenance of the unborn
child during the entire period of gestation
- birth of the child and expulsion of the
placenta, and
- Suckling
and care of the child, with an eventual return of the maternal organs to
virtually their original state.
Human beings exhibit sexual reproduction and vivipary.
Like all mammals human beings are unisexual with either the
male or female reproductive system.
Of the reproductive structures, the gonads (testes in males
and ovaries in females) are considered as the primary sex organs, while other
associated structures including reproductive ducts and glands are known as
secondary sex organs.
Table 1: Secondary sex organs
Male
|
Epididymis, vasa deferens, prostrate, seminal vesicles,
penis
|
Female
|
Fallopian tubes, uterus, vagina, mammary glands
|
Human beings also exhibit sexual dimorphism, i.e. male and
female exhibit certain specific morphological features make them distinct from
the other sex. These characters are known as secondary or accessory sexual
characters, and the phenomenon is known as Sexual
Dimorphism.
Basic Phases of reproductive
physiology:
The reproductive events in humans include:
- Gametogenesis: Formation of
gametes.
Male gametes or Sperms
and female gametes or ova (singular
ovum), are haploid sex cells formed from diploid germ cells. The germ cells are
present in primary reproductive organs called gonads. Gonads in male are testes
and in females are ovaries.
Gametogenesis in males involves formation of sperms – Spermatogenesis
Gametogenesis in females involves formation of ova – Oogenesis
- Insemination: Transfer of sperms
in to female genital tract
- Fertilization: Fusion of male and
female gametes to form diploid zygote
- Implantation: Involves 2 steps.
First, rapid cell division of zygote leads to formation of single layered
hollow spherical larva called blastula.
The process is known as blastulation.
Next the blastula becomes attached
to the endometrium of uterine wall. This step is known as implantation.
- Gestation: Embryonic development.
It involves:
- Placentation: involves the
formation of an intimate physiological and mechanical connection between
the foetal and maternal tissues to enable nutrition, respiration, and
excretion etc of the fetal tissue.
- Gastrulation: Formation of
gastrula larva from the blastocyst. Gastrula larva has three primary germ
layers.
- Oganogenesis: Formation of
specific organ system from the three germ layers.
In humans the gestation period is of 280 days.
- Parturition: Child delivery of the
fully formed human baby.
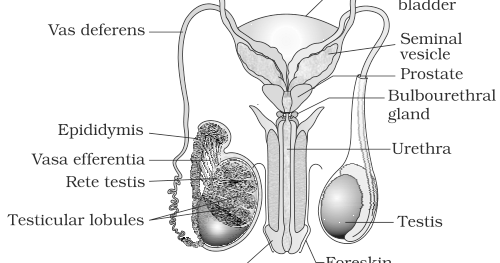
MALE REPRODUCTIVE SYSTEM
Located in pelvis region
Comprises of:
- A
pair of testes
- Accessory
ducts
- Glands
and
- External
genitalia
I.
Testes: Primary
sex organ.1 pair.
Oval, 4-5cm in length, 2-3 cm in
width
Situated below the abdominal cavity
within a pouch known as scrotum or
scrotal sacs
The scrotal sacs are filled with a tissue
fluid called hydrocoel. Gubernaculum
and spermatic cord keep the testes
in position inside the scrotal sacs.
Scrotal sacs help in maintaining
the low temperature of the testes (at 2-2.5 deg C lower than the normal
internal body temperature. This is important for normal; spermatogenesis
since high body temperature kills spermatogenic tissue.
Each testis is covered by a dense
white fibrous capsule known as tunica albuginea. It projects inside the testes as fibrous
septa. The septa divide the testis into 250 compartments called testicular lobules.
Each of the testicular lobule has 1-3
highly coiled seminiferous tubules. The
seminiferous tubules produce sperms. The seminiferous tubules are lined on
the inside by two types of cells:
·
Male germ
cells or Spermatogonia: produce sperms
·
Sertoli or
nurse cells: Provide nutrition to germ cells
The germ cells undergo meiotic
divisions and form haploid and motile gametes known as spermatozoa.
The
region in between the seminiferous tubules is known as interstitial spaces. It contains small blood vessels and interstitial cells or leydig cells. Leydig
cells synthesize and secrete testicular hormone called androgens. The most
important androgen is testosterone, this
controls the development of secondary sexual characters and spermatogenesis.
Function
of testes: spermatogenesis and secretion of testosterone
II.
Accessory
ducts: the male sex accessory ducts include
a.
Rete Testis
b.
Vasa
efferentia
c.
Epididymis
d.
Vasa
deferentia
Seminiferous tubules open into a
network of tubules known as rete testis
which further leads in to vasa efferentia.
The vasa efferentia leaves the testes and opens in to epididymis on the posterior surface of each
testis.
The main function of epididymis is conduction of sperms by
peristalsis. Epididymis also helps in storage nutrition and physiological
maturation of sperms by removing certain decapacitation factors.
Epididymis leads to vasa deferens that ascends to the
abdomen and loops over the urinary bladder. It receives a duct from the seminal
vesicle and opens in to urethra as the
ejaculatory duct.
III.
Urethra: arises
from the urinary bladder, joins the ejaculatory duct to form the urinogenital tract. It extends through
the penis. This tract carries urine, sperms and secretions of seminal vesicles,
Cowper’s glands.
IV.
Penis: male
external genitalia
Made of special tissue that helps
in erection of the penis to facilitate insemination. Tip of penis is highly
sensitive and enlarged. It is called glans penis. The tip of glans penis
is covered by a loose retractile skin known as foreskin. Glans also has
a slit like opening of urinogenital tract called urethra maetus.
V.
Male
Accessory Gland: Include
·
Seminal
vesicle: secretions comprise 60-70% of semen. Mainly formed of fructose,
citrate, several proteins and prostaglandins. Activate spermatozoa and
stimulate vaginal contractions to help in fusion of gametes.
·
A
Prostrate gland: Surrounds the proximal part of urethra. Pours alkaline
secretions in urethra. Secretions contain lipids, small amount of citric acid,
bicarbonate ions and some enzymes e.g. fibrinolysin.
It forms 20% of semen. Main
functions are:
o Activates
sperms
o Provides
nutrition to sperms
o Neutralizes
acidity of urine
o Adjusts
vaginal pH
·
A pair of
bulbourethral glands: secretes mucus like alkaline substance which provides
lubrication to penis.
Secretions of these glands constitute
the seminal plasma which is rich in fructose, calcium and certain other
enzymes.
Thus the major functions of male
reproductive system include:
ü
Spermatogenesis
ü
Secretion
of male hormone testosterone
ü
Transfer
of sperms to female reproductive system for fertilization of ovum
FEMALE
REPRODCUTIVE SYSTEM
FIGURE 3.3
Located in pelvis region
Comprises of:
·
A pair of ovaries
·
A pair of oviducts
·
uterus
·
cervix
·
vagina
·
external genitalia
Fallopian tubes, uterus and vagina collectively form the
accessory ducts.
The above organs along with mammary glands are together
involved in the reproduction which includes the following processes:
o ovulation
o fertilization
o pregnancy
o birth
and
o child
care
1. Ovaries:
Primary female sex organs, produce ovum and several steroid hormones (ovarian
hormones)
o 1
pair, small sized (2-4 cm), almond shaped
o present
in pelvis region, one on each side of uterus
o suspended
from abdominal wall by mesovarium
o attached
to pelvic wall and uterus by ovarian
ligament
Each ovary is covered by a thin germinal epithelium. The
epithelium surrounds the stroma that is divided in to 2 zones:
- Outer
Cortex
- Inner
medulla
In the medulla of ovaries are
present a number of developing or primary ovarian follicles in different stages
of oogenesis.
Cortex may contain either a yellow
conical endocrine gland known as corpus
luteum or a degenerating white corpus
albicans.
2. Fallopian
tubes or Oviducts: each is 10-12 cm long, and extends from periphery of each
ovary to the uterus.
The fallopian tubes comprise of 3 parts:
a. Infundibulum: Part closer to ovary is funnel shaped infundibulum. The ends of infundibulum
have finger like projections known as fimbriae.
Fimbriae help in collection of ovum after ovulation.
b. Ampulla: The infundibulum leads to a wider ampulla.
c. Isthumus: The ampulla leads the last part of oviduct which
has a narrow lumen and leads in to uterus. It is ciliated.
Ampullary isthmic junction is the site of fertilization
3. Uterus
or Womb: single, inverted pear shape, muscular and highly vascular. Supported
by ligaments attached to the pelvic wall.
Formed of three parts:
·
Fundus: upper dense part
·
Body or corpus: middle and main part. The wall
of uterus in this region is made of three layers.
Table 2: Uterine wall layers
and their functions
Perimetrium
|
External, thin and membranous
|
Forms envelope
|
Myometrium
|
Middle thick layers of smooth muscles
|
Helps in child birth by undergoing strong contractions
|
Endometrium
|
Inner and Glandular layer
|
Undergoes cyclical changes during menstrual cycle
Site of implantation and foetal growth during pregnancy
Sit of formation of placenta
|
·
Cervix: lower narrow part. Uterus opens in to
vagina through cervix. Cavity of cervix known as cervical canal, which along with vagina forms the birth canal.
4. Vulva:
external genitalia of the female. It comprises of:
·
Vestibule
or a depression that has two apertures: upper urethral orifice and a lower vaginal
orifice. The vaginal orifice is partially covered by a membranous fold
called hymen which is torn either
during the first coitus, or due to an incident of sudden fall, jolt, physical
activity such as sports, horse riding, cycling, or during insertion of tampons.
In some women hymen may persist even after coitus.
·
Vestibule is bounded by two pairs of moist
fleshy skin folds with sebaceous glands: inner smaller labia minora and outer larger labia
majora.
·
The labia minora fuse anteriorly to form a skin
fold known as prepuce which lies in
front of a small erectile organ glans
clitoris (homologous to penis).
·
A fleshy elevation is present above labia
majora, known as mons pubis. It is
covered by skin and pubic hair.
5. Mammary
Gland: A functional mammary gland is a characteristic feature of mammals.
Mammary glands are paired
structures, containing glandular tissue and fats.
The glandular tissue is divided
in to 15-20 mammary lobes containing
clusters of cells known as alveoli. The
cells of alveoli secrete milk, which is stored in the lumen of alveoli.
The alveoli open into mammary tubules. The mammary tubules
join to collectively form mammary duct. Several mammary ducts join to form
wider mammary ampulla. The mammary
ampulla is connected to lactiferous duct
through which milk is sucked out.
The uterus, oviducts,
vagina, clitoris, the accessory genital glands and the mammary glands are
referred to as secondary sex organs of female.
Major Functions of Female Reproductive System
- Oogenesis
by germ cells of ovary
- Receiving
seminal fluid
- Fertilization
of gametes to form zygote
- Implantation
followed by prenatal growth
- Parturition
- Post
natal care
Gametogenesis
Process of formation and differentiation of haploid gametes
(sperms and ova), from diploid primary germ cells (gametogonia)
The gametogonia (spermatogonia and oogonia) are present in
primary sex organs or gonads; testes in male and ovaries in female.
Thus gametogenesis can be of 2 types:
- Spermatogenesis
- Oogenesis
Spermatogenesis
Formation of haploid and
functional male gametes (spermatozoa, n) from diploid reproductive cells,
spermatogonia (2n) present in testes of male organism.
Occurs in testes
Begins at puberty
Continuous process completed in 74
days
Process: Divided in to 2 phases:
- Formation of Spermatids:
- Multiplicative
or mitotic phase: The spermatogonia (2n) present on
the inside wall of seminiferous tubules multiply by mitotic division and
increase in number. Each spermatogonium is diploid and contains 46
chromosomes.
- Growth
Phase: Diploid
- Some
of these spermatogonia called primary spermatocyte
periodically undergo meiosis. A primary spermatocyte completes first
meiotic division (reduction division) leading to formation of two equal
haploid cells called secondary spermatocyte, which
have only 23 chromosomes.
- The
secondary spermatocytes (n) undergo second meiotic division to produce
four equal haploid spermatids (n).
- Spermatids
are non-motile.
- Spermiogenesis
i.
The spermatids are transformed into spermatozoa (sperms,
n) by the process called spermiogenesis.
Spermiogenesis converts the non motile spermatids in to functional and
motile spermatozoa.
The main aim of spermiogenesis is to
increase sperm motility by reducing weight and development of locomotory
structure.
ii.
After spermiogenesis, sperm heads become embedded in
sertoli cells which provide nourishment to them.
iii.
Mature spermatozoa are finally released from
seminiferous tubules by the process called spermiation.
Sperms once released from seminiferous tubules, are
transported by accessory ducts. Secretion of epididymis, vas deferens, seminal
vesicle, and prostrate are essential for maturation and motility of sperms.
Thus:
Sperms+Seminal Plasma=Semen
The functions of male sex accessory ducts and glands are
maintained by the testicular hormones (androgens).
Structure of Sperm
Ø
Microscopic
Ø
Composed of Head,
Neck, Middle piece and a Tail
Ø
A plasma membrane envelops the whole body
Ø
Head contains
an elongated haploid nucleus. Its anterior part is covered by a cap like
structure called acrosome.
Acrososme is formed from a part
of the Golgi Body of the spermatid. It is filled with enzymes that help
fertilization of the ovum. The lytic enzyme hyaluronidase present in acrosome is responsible for penetration of
ovum during sperm entry.
Ø
The middle piece has many mitochondria. They
produce energy required for the movement of tail that causes sperm motility.
Sperm motility is essential for fertilization.
Ø
Tail is the longest part of sperm. It exhibits
lashing movements that provide forward push to the sperm.
A human male ejaculates about 200 to 300 million sperms
during coitus of which for normal fertility at least 60% sperms must have
normal shape and size; and at least 40% must have normal motility.
Viability of human sperm is 24 hours.
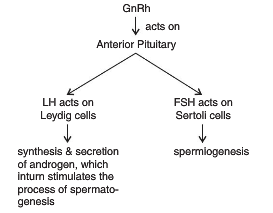
Control
Spermatogenesis starts at the age of puberty due to
significant increase in secretion of gonadotrophin releasing hormone (GnRH).
It is a hypothalamic hormone.
High level of GnRH acts on anterior pituitary and stimulates
release of 2 gonadotrophins:
- Leutinising
Hormone (LH): Acts at Leydig cells and stimulates synthesis and secretion
of androgens.
Androgens stimulate process of
spermatogenesis
- Follicle
Stimulating Hormone (FSH): acts on Sertoli cells, and stimulates secretion
of some factors which help in process of spermiogenesis.
Control of Spermatogenesis
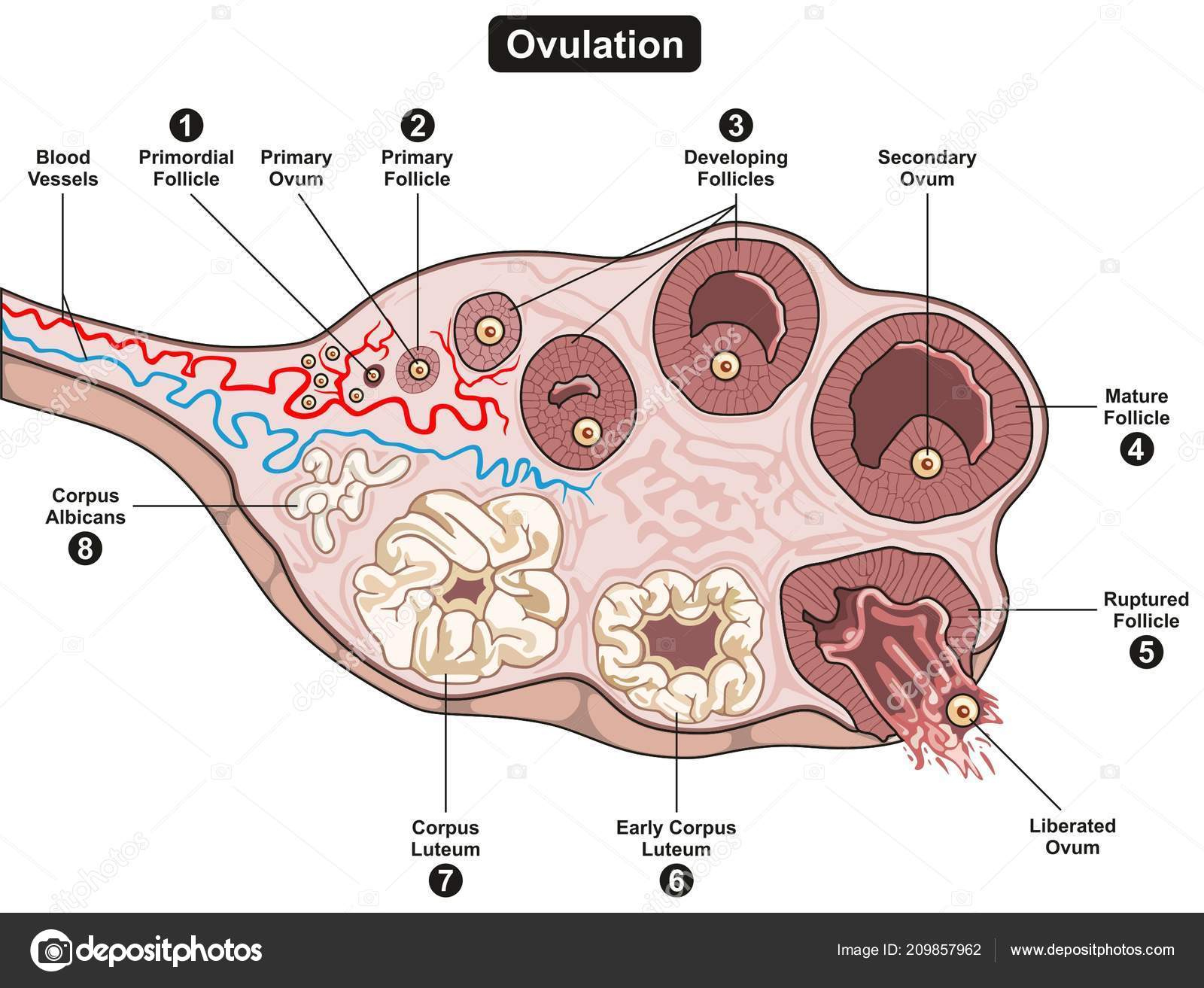
Oogenesis:
Process of formation of natural haploid female gamete called
ova (n) (singular: ovum), from diploid egg mother cells Oogonia (2n) of ovary.
Initiated during embryonic development stage. A couple of
million gamete mother cells are formed within each foetal ovary. No more are
formed and added after birth.
The process involves three phases:
- Multiplicative
Phase: Certain primary germ cells of the germinal epithelium of ovary
undergo rapid mitotic divisions to form groups of diploid egg mother cells or oogonia (2n).
- Growth
Phase: The oogonium start division and enter prophase I of meiosis. The
division gets arrested at that stage forming primary oocyte.
- Each
primary oocyte then gets surrounded by layer of granulosa cell and is
then called Primary Follicle. Many
of these primary follicles degenerate during the phase from birth to
puberty. By puberty only about 60,000 – 80,000 primary follicles remain
in each ovary.
- Each
Primary follicle then gets surrounded by more layers of granulosa and a
theca forming the secondary
follicle.
- Secondary
follicle than develops a fluid filled antral cavity called antrum and is now termed as Tertiary Follicle. The theca
layer gets organized in to inner theca
interna and outer theca
externa.
- Maturation
Phase:
- At
this stage the primary oocyte within the tertiary follicle grows in size
and completes its first meiotic division. It is an unequal division
resulting in formation of a large secondary
oocyte and a tiny first Polar
Body.
- The
secondary oocyte retains bulk of the nutrient rich cytoplasm of the
primary oocyte.
- The tertiary follicle further
changes into Graffian Follicle.
- The
secondary oocyte forms a new membrane called Zona Pellucida surrounding it. The Graffian Follicle now
ruptures to release the secondary oocyte (Ovum) from
the ovary by the process called Ovulation.
Structure of Ovum
- Maternal
haploid gamete
- Generally
spherical, non motile with yolky cytoplasm enveloped in 1 or more egg
envelopes
- Human
ovum is alecithal with negligible amount of cytoplasm
- Cytoplasm
is differentiated in to outer, smaller and transparent exoplasm or egg cortex; and inner larger and opaque endoplasm or ooplasm
- Nucleus
is large and excentric
- The
side of ovum with nucleus and polar body is known as Animal Pole; and the opposite side is known as Vegetal Pole.
- Ovum
is surrounded by many egg envelopes:
- Vitelline
Membrane: inner, thin and transparent
- Zona
Pellucida: middle, thick and transparent
- Corona
Radiata: outer and thick
Spermatogenesis vs. Oogenesis
Menstrual Cycle:
The cyclic changes that occur in the reproductive organs of
primate females is called menstrual cycle.
Menarche: The
beginning of first menstruation at puberty.
Menopause: Menstrual
cycle cease at the age of 45 – 50. This is known as menopause.
In human females the menstruation is repeated at an average
interval of 28/29 days. The entire cycle starting from one menstruation to
next, is known as menstrual cycle. The cycle involves the release of an ovum
during the middle of the cycle.
There are typically 4 phases
in menstrual cycle, controlled by two types of hormones: follicle stimulating
hormones (FSH) and luteinising hormones (LH).
Menstrual phase
It lasts for 3-5 days
It results due to breakdown of endometrial lining of uterus
and its blood vessels
Menstruation occurs only if fertilization of the ovule does
not take place. Lack of menstruation may be indicative of ovule fertilization
and hence of pregnancy. However, it may also be due to stress, poor diet, poor
health etc.
Follicular phase
Primary follicle in the ovary grow to become a fully mature
Graffian follicle. Simultaneously, Endometrium is regenerated by proliferation
of its cells
These changes are due to increased levels of pituitary and ovarian hormones: Gonadotropins
(FSH, LH), Estrogen
FSH controls follicular phase, stimulates growth of
follicles.
Secretion of FSH and LH, increases gradually during the follicular
phase. It performs 2 functions:
- Stimualtes
follicular development
- Stimulates
secretion of estrogen by growing follicles
Secretion of Estrogen occurs during the follicular phase.
Ovulatory phase
Involves ovulation. Ovulation of
mature follicles on the ovary is induced by a large burst of LH secretion known
as the preovulatory LH surge
Peak level of LH induces rupture of mature Graafian follicle
and release of ovum or ovulation.
Luteal phase
Ruptured follicle transforms into corpus luteum
Residual cells within ovulated
follicles proliferate to form corpora luteum, which secrete the steroid
hormones progesterone and estradiol. Progesterone is necessary for maintenance
of pregnancy by maintaining endometrium. In most mammals, LH is required for
continued development and function of corpora luteum. [The name luteinizing hormone derives from this effect of
inducing luteinization of ovarian follicles.]
During pregnancy, all events of all events of menstrual
cycle stop and there is no menstruation.
In absence of fertilisation, corpus luteum degenerates. This
causes disintegration of endometrium leading to menstruation, marking the
beginning of a new cycle.
Fertilisation and Implantation
The process of fusion of a sperm with an ovum is called fertilisation.
Fertilisation can only occur if the ovum and sperms are transported
simultaneously to the ampullary – isthmic junction.
Events during fertilisation:
- 200-300
million sperms are introduced in to female genital tract.
- About
50% of these are killed due to acidity in the female genital tract.
- Many
are engulfed by the phagocytes of the vaginal epithelium.
Thus around 100 sperms only reach the fallopian tubes.
- Ovulation
or release of ovum from graffian follicle of the ovary occurs on the 14th
day. At the time of ovulation, the
ovule is at secondary oocyte stage.
- Penetration
of Sperms: Sperm comes in contact with egg at animal pole. Sperm
penetration is a chemical phenomenon. Acrosome of sperm comes in contact
with zona pellucida. Acrosome releases certain sperm lysins that dissolves
egg envelope locally and thus make path for penetration of sperm. The lysing enzyme present in sperm
lysins is Hyaluronidase. It penetrates through corona
radiate and dissolves zona pellucida.
Only the sperm nucleus and middle
piece enter the ovum, the tail is lost.
- In
humans there is always monospermy.
Entry of sperm induces changes in membrane that block entry of additional
sperms
- Entry
of sperm induces:
- Meiotic
division of secondary oocyte to form haploid ovum and 2nd polar body.
- Formation
of zygote
Significance of
fertilization:
i.
Stimulates the secondary oocyte to undergo second
maturation division to release second polar body and to form haploid ovum.
ii.
Restores diploidy
iii.
Fertilization membrane prevents polyspermy
iv.
Combines characters of two parents and introduces
variations. So helps in evolution
v.
Centrioles of sperm from the spindle to initiate the
cleavage of zygote
Cleavage
Rapid mitotic division of zygote to from hollow, spherical
multicellular developmental stage called blastula.. So the process is also
called bl;astulation.
Ø
Formation
of Morula
- In
human zygote cleavage occurs in fallopian tubes during the passage of
zygote towards the uterus.
- It
is holoblastic,
radial, indeterminate and unequal.
- The
zygote divides first in to 2 unequal cells called blastomeres.
- Second
cleavage is perpendicular to first.
- Subsequent
divisions occur rapidly one after the other leading to formation of Morula.
- Morula
is 16-32 cell stage
Ø
Formation
of Blastula
·
Rearrangement of Blastomeres
·
Outer layer of cells becomes flat and forms
trophoblast, that draws nutrition from endometrium of uterus
·
The inner cell mass is known as micromeres.
·
The central cavity is known as blastocoel, in
which the nutrition collects.
Implantation
Process of attachment of blastocyst on the endometrium of
uterus
Blastocyst gets embedded in endometrium of uterus (implantation)
Uterine cells rapidly divide and cover the blastocyst
Implantation may occur anytime between 6th and 10th
day after fertilization (usually 7th day)
Pregnancy and embryonic development
Inner layer grows out as finger like projections called
villi into the uterine stroma
Chorionic villi and uterine tissue get interdigitated to
form placenta
Placenta secretes hormones like hCG , hPL , estrogens ,
progesterones (to maintain pregnancy)
Inner cell mass differentiates into an outer layer called
ectoderm and an inner layer called endoderm
Mesoderm appears between ectoderm and endoderm
Stem cells (undifferentiated embryonic cells)
Features of embryonic development
The human pregnancy lasts for 9 months
1st month – embryo’s heart is formed
2nd month – foetus develops limbs and digits
12 weeks (1st trimester) – major organ systems are formed
5th month – 1st movements of foetus and appearance of hair
on head
24 weeks (2nd trimester) – body covered with fine hair , eye
lids separate , eye lashes formed
Parturition and Lactation
Gestation period – 9 months
Parturition – the process of delivery of the foetus
(childbirth)
Signals for parturition originate from the fully developed
fetus and placenta inducing mild uterine contractions called Foetal
ejection reflex
It triggers the release of oxytocin from maternal pituitary
Oxytocin acts on uterine muscle, causes stronger
uterine contractions, which in turn stimulates further secretion of oxytocin.
Lactation
The mammary glands undergo differentiation during pregnancy
and starts producing milk towards the end of pregnancy by the process called
lactation.
The milk produced during the initial few days of lactation –
colostrum
It contains several antibodies essential to develop
resistance for new-borns.